NCCCP is pleased to present this peer-reviewed article, which was researched and written by pharmacy students at the University of the Pacific.
The Analgesic Efficacy of IV and IM Ketorolac: A Systematic Review
Timofey Shimko, Chiron Tran, Sophia Wong, Allyson Chan, Anthony Bao, Samantha Seto
- Abstract
This systematic review aimed to determine whether parenteral doses of ketorolac reach a ceiling in analgesic efficacy at doses lower than those recommended in the FDA-approved labeling. This question is of clinical importance because of ketorolac’s serious dose-dependent side effects. If lower, off-label doses of ketorolac prove to be sufficient to meet equivalent analgesic targets, then this may justify the use of those doses in patients at higher risk for experiencing ketorolac adverse effects. Out of an initial selection of 1,196 articles and clinical trial publications, 14 were selected for analysis: eight trials comparing intravenous (IV) ketorolac in varied doses and five trials comparing intramuscular (IM) ketorolac in varied doses. Of the 14 publications, ten featured an active control while the other four were placebo-controlled. One trial directly compared the same dose of IV and IM ketorolac. Our analysis of these 14 publications found varying results, with effective analgesic ceilings ranging from 10–30 mg for both the IV and IM formulations of ketorolac.
- Introduction
Ketorolac is a non-steroidal anti-inflammatory drug (NSAID) first introduced in 1989. It was the first NSAID approved for parenteral use and can be administered by various routes: oral, intravenous, intramuscular, ophthalmic, and intranasal (Vadivelu 2017). Parenteral ketorolac is FDA-approved for treating pain severe enough to require opioid-level analgesia, such as during and after surgery. Among the 14 publications analyzed in this review, the cohorts studied included patients receiving ketorolac for cancer-related pain, post-operative pain, musculoskeletal pain, kidney stones (renal colic), acute pain of unspecified etiology, and perioperative use to reduce post-surgical pain or the need for post-surgical opiates.
Like other NSAIDs, ketorolac increases the risk of bleeding, cardiovascular events (such as myocardial infarction and stroke), and peptic ulcers. Of interest, several studies have documented that ketorolac is associated with a higher risk for upper gastrointestinal complications compared to other NSAIDs (García Rodríguez 1998, Castellsague 2012). These risks contributed to ketorolac’s boxed warning that it should not be used for more than 5 days. Therefore, it is important to use the lowest dose necessary to minimize ketorolac’s potential risks. Studies have observed analgesic ceilings for other NSAIDs, including ibuprofen, ketoprofen, and zomepirac (Laska 1986, Seymour 1996, Eisenberg 1994). Recently, there has been a renewed interest in determining the analgesic ceiling of ketorolac (Motov 2017, Yurashevich 2020, Eidinejad 2020) especially due to growing interest in opioid stewardship and non-opioid pain management. According to the FDA label, the medication is dosed at 30 mg IV and 60 mg IM for patients under 65, given as single doses (Ketorolac tromethamine FDA label). A multi-dose regimen may also be administered; however, we chose to study the single-dose regimen to ensure ease of comparison and avoid the introduction of confounding variables. This systematic review will review the similarities and differences between IV- and IM-administered ketorolac, the two most common routes of administration in practice today (Soleyman-Zomalan 2017).
- Methods
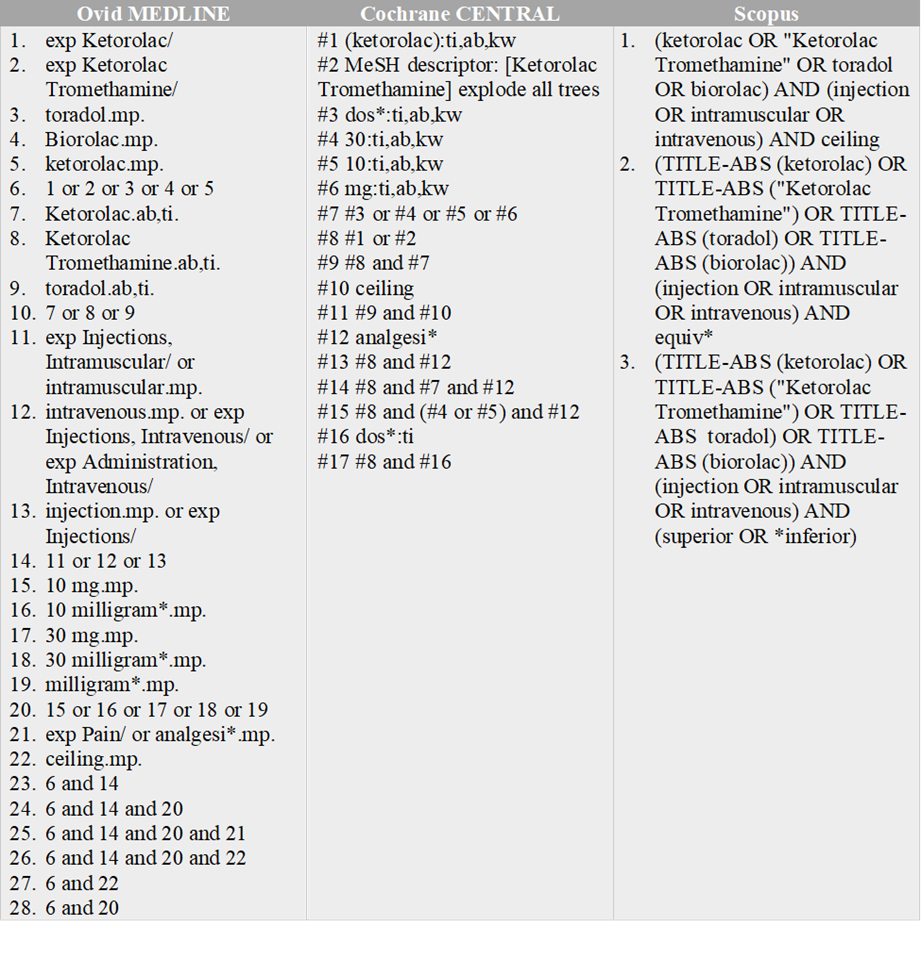
3.1. Data sources
A comprehensive search strategy was developed to find relevant studies from published and unpublished literature. The search strategy can be found in the appendix. The following databases were searched for articles: MEDLINE (via Ovid), searched from 1946 to 2 June 2022; Cochrane Central Register of Controlled Trials (CENTRAL; via the Cochrane Library), searched on 2 June 2022; and Scopus, searched on 2 June 2022.
3.2. Study eligibility and selection
Eligible studies included randomized controlled trials (RCTs), non-RCTs, and observational studies that focused on the analgesic efficacy of IM and IV ketorolac at various doses in patients experiencing pain (additional details outlined in Appendix A). The type of pain (e.g., renal colic, post-operative pain, etc.) did not affect the selection process. In the first round of article screening, the initial pool of articles was divided based on date into six different groups, with each group being assessed by a separate reviewer to determine relevance based on a review of abstracts. Rayyan (https://rayyan.ai), a web-based organization tool for systematic study review, was used to facilitate this process. The titles and abstracts of each article were considered for article selection. After this initial selection of articles, full texts were reviewed to refine the selection further and remove articles that failed to meet inclusion or satisfied exclusion criteria.
3.3. Data extraction
The following pieces of information were extracted from each of the selected articles: number of participants in the study, the dosing and formulation of ketorolac, dosing regimen, study duration, analgesic outcome measures and results, and intervention for adverse effects. A complete list of the extracted information can be found in Appendix A.
3.4. Study quality assessment
Each article was analyzed for bias, including selection bias, performance bias, detection bias, attrition bias, reporting bias, and study size. The criteria for low, high, and unknown risk of bias are listed in Figure 1.
| Low risk | High risk | Unknown risk | |
| Random sequence generation (selection bias) | Groups formed by any truly random process | Non-random method was used | Randomization method was not stated |
| Allocation concealment (selection bias) | Allocations conducted using telephone randomization, sealed/opaque envelopes, or another low-risk allocation method | Open list was utilized | Concealment method was not disclosed |
|
Blinding of participants and personnel (performance bias)
|
Participants and personnel both blinded | No blinding was incorporated into the study | Blinding not clearly described |
| Blinding of outcome assessment (detection bias) | Assessors were blinded, and a method of blinding was explained | Assessors were not blinded | Method of blinding was not clearly stated |
| Incomplete outcome data (attrition bias) | If less than 10% of the participants failed to complete the study or if a “baseline observation carried forward” analysis was used | If the study included results from only participants who completed the study | If a “last observation carried forward” analysis was utilized |
| Selective reporting (reporting bias) | All planned outcomes mentioned in the methods were reported | Some outcomes were reported which were listed in the methods, but not all | No distinction between outcomes that were planned and reported |
| Sample size | More than 200 participants were studied per treatment arm | 50-199 participants were studied per treatment arm | Less than 50 participants were studied per treatment arm |
Figure 1. Criteria used to assess Risk of bias
- Results
4.1. Literature search/screening
Our initial literature search yielded 1196 references from MEDLINE, CENTRAL, and Scopus. After reviewing the titles and abstracts of these references, we identified 455 potentially relevant studies and excluded 741 irrelevant and duplicate studies. After a second round of screening, we excluded another 441 studies that met our exclusion criteria or did not meet our inclusion criteria.
Figure 2. Study flow diagram
4.2. Included studies
Fourteen studies fulfilled our inclusion criteria of comparing the analgesic efficacies of different IM and IV ketorolac doses given as a single administration: Duttchen 2017, Eidinejad 2020, Fosland 1990, Khadge 2020, Minotti 1998, Motov 2017, O’Hara 1987, Parke 1995, Shanechi 2018, Turner 2021, Yee 1986, Yoon 1995, Yurashevich 2020, and Zhou 2001. All the studies compared ketorolac with itself at different doses. Eight studies investigated IV ketorolac (Duttchen 2017, Eidinejad 2020, Khadge 2020, Motov 2017, Shanechi 2018, Yoon 1995, Yurashevich 2020, and Zhou 2001) while five other studies featured IM ketorolac (Folsland 1990, Minotti 1998, O’Hara 1987, Turner 2021, and Yee 1986). Only one study focused on both IM and IV ketorolac (Parke 1995). The study designs, treatment groups, outcome measures, and results for each of these studies are specified in Appendix A.
4.3. Excluded studies
441 studies did not meet our inclusion criteria (Figure 2). Common reasons for exclusion were studying only one strength of ketorolac, lack of relevance, or administration of ketorolac by non-parenteral routes (refer to Figure 2 for the complete list of reasons).
4.4. Risk of bias in included studies
Figure 3. Assessed risk of bias in each study
4.5. Results
4.5.1. IV Ketorolac
4.5.1.1. Eidinejad 2020
- At the 30-minute mark, the different doses of ketorolac (10, 20, and 30 mg) were non-inferior to one another.
- There was no statistically significant difference between the 3 groups in pain reduction at the 15, 45, and 60 minute marks.
- Adverse effects occurred less frequently in the 10 mg group, but the difference was not statistically significant.
- The need for a rescue analgesic was similar for all three groups.
4.5.1.2. Motov 2017
- Pain reduction in each of the treatment arms (10, 15, and 30 mg) 30 minutes after ketorolac administration was not significantly different.
- Similarly, the change in pain scores recorded at other time points (the 15, 60, 90, and 120 minute marks) was not significantly different between the three doses.
- No differences were observed between the groups regarding morphine use.
- There were no significant differences in the incidence of adverse effects reported in each of the treatment arms.
4.5.1.3. Shanechi 2018
- No significant difference in the degree of pain relief was observed at any time between three doses of ketorolac (10, 15, and 30 mg) 30 minutes after IV administration.
- No clinically significant differences were observed regarding the frequency of adverse effects and the need for rescue medication (see appendix for the study’s definition of clinical significance).
4.5.1.4. Yurashevich 2020
- No significant difference was observed between the treatment groups (15 and 30 mg) regarding opioid use.
- Opioid use 24 and 48 hours post-delivery, average pain scores after six hours, number of patients with serum creatinine greater than 0.9 mg/dL and the use of rescue antiemetic medication within the first 48 hours were not significantly different between the treatment arms.
4.5.1.5. Khadge 2020
- The need for postoperative opioid administration was not significantly different between the two treatment arms (15 and 30 mg).
- While a significant difference in baseline pain score was observed when comparing the 15 mg and 30 mg treatment groups, there was no significant difference in the baseline pain scores of the 15 mg and placebo (0 mg) groups.
4.5.1.6. Yoon 1995
- While the placebo (normal saline) and the ketorolac 10 mg dose were both ineffective at providing analgesia, all doses of ketorolac above 15 mg (30, 45, and 60 mg) had analgesic effects that did not increase with increasing doses of ketorolac.
- No adverse events were observed in any of the participants.
4.5.1.7. Zhou 2001
- Pain relief between treatment arms (15 and 30 mg) was not significantly different.
- There were no significant differences related to adverse effects reported in each of the treatment groups.
4.5.1.8. Duttchen 2017
- Non-inferiority in analgesic efficacy was not confirmed between the 15 and 30 mg doses when pain was evaluated four hours after administration.
- There was a nonsignificant difference between the two groups in terms of morphine usage both 8 hours and 24 hours after the operation.
- Side effects occurred more frequently in the 30 mg treatment group compared to the 15 mg group.
4.5.2. IM Ketorolac
4.5.2.1. O’Hara 1987
- The 30 and 90 mg doses were observed to reduce pain by a similar intensity and were both more effective at providing analgesia compared to the 10 mg dose.
- No significant differences were observed in the number of side effects that occurred in each of the treatment groups.
4.5.2.2. Turner 2021
- The 15 and 60 mg doses reduced pain to similar degrees when evaluated both 30 and 60 minutes after dose administration.
- A significantly higher incidence of adverse effects was documented in the 60 mg treatment group as opposed to the 15 mg group.
4.5.2.3. Minotti 1998
- The 10 mg and 30 mg doses reduced pain in a manner that was not significantly different three and six hours after administration.
- Out of the two groups of 60 patients receiving the 10 mg and 30 mg doses, adverse effects were only experienced by two patients from each group.
4.5.2.4. Folsland 1990
- Pain relief for 30 mg ketorolac during eight hours was superior to 10 mg ketorolac and the placebo, while the 10 mg dose was only statistically superior at the 0-6 hour intervals.
- Regarding side effects, more were observed for patients given the 10 mg dose (seven recorded instances of mild and moderate side effects) than the 30 mg dose (two recorded instances of mild and moderate side effects).
4.5.2.6. Yee 1986
- The investigators concluded that the 10 and 30 mg doses were similar in analgesic efficacy, while the 90 mg doses tended to be superior in efficacy than the former two doses.
- Regarding side effects, no significant difference was observed in the reported frequency for all three doses.
4.5.3. IM & IV Ketorolac
4.5.3.1. Parke 1995
- The investigators concluded that IV administration of ketorolac did not confer any advantages over the IM route in terms of efficacy or onset of action.
- There were no significant differences in the adverse effect profiles of IM and IV ketorolac.
- Discussion
The primary objective of this systematic review was to confirm the existence of an analgesic ceiling for the IV and IM formulations of ketorolac in addition to clarifying the doses at which this ceiling effect occurs. This review also aimed to determine whether or not there is a difference in adverse events between the two dosage forms. Starting with IV ketorolac, the articles included in our review overall demonstrate an analgesic ceiling lower than the maximum dose currently recommended by the FDA. Recent studies such as Eidenejad 2020, Motov 2017, and Shanechi 2018 have used various pain assessment tools to assess the analgesic efficacies of different IV ketorolac doses; however, despite these differences, all three studies concluded that ketorolac 10 mg IV was non-inferior to higher doses of IV ketorolac in terms of pain relief. Similarly, other studies such as Khadge 2020, Yoon 1995, Yurashevich 2020, and Zhou 2001 concluded that the analgesic ceiling for IV ketorolac was 15 mg. That being said, it should be noted that Khadge 2020, Yurashevich 2020, and Zhou 2001 did not investigate ketorolac at doses lower than 15 mg IV, thereby indicating that these two conclusions are not entirely inconsistent with one another.
In contrast to these findings, two studies showed what appeared to be a greater analgesic effect with higher study doses. One of these, Yoon 1995, studied various doses of IV ketorolac, including a 10 mg and 15 mg dose. The 10 mg dose was observed to be inferior in its analgesic efficacy to the 15 mg dose based on observation alone. The other, Duttchen 2017, which studied 15 mg and 30 mg IV ketorolac, was unable to demonstrate non-inferiority of the 15 mg dose compared to the 30 mg dose. However, it is important to note that both of these studies had relatively small treatment groups (mean: 19) compared to the other studies that were analyzed in this review (mean: 153).
Moving onto IM ketorolac, there was significantly more heterogeneity between the studies included in this review in terms of the observations and conclusions that were made about the efficacies of different IM ketorolac doses. Only one study investigated the FDA-approved IM ketorolac dose of 60 mg and compared it to a lower dose of 15 mg IM, which the investigators concluded was non-inferior to the 60 mg dose in terms of analgesic efficacy (Turner 2021). Two studies determined a lower 10 mg dose was similar in analgesic efficacy to the 30 mg dose (Minotti 1998 and Yee 1986). Yee 1986, however, concluded that the 90 mg dose was statistically superior to the 10 and 30 mg doses.
In contrast to this conclusion, O’Hara 1987 determined that the 30 mg dose was non-inferior to the 90 mg dose, while the 10 mg dose was inferior to both. Finally, Folsland 1990 concluded that the 10 mg dose was inferior to the 30 mg dose. Based on these conclusions, it is more reasonable to suggest that the analgesic ceiling for IM ketorolac is 30 mg instead of 10 or 15 mg. It should be noted that Folsland 1990, O’Hara 1986, and Yee 1986 had fairly small treatment groups (mean: 36) and were at high risk for bias regarding sample size. Greater sample sizes may have resulted in less variability in the results. Regarding the study that directly compared IV and IM ketorolac, the investigators concluded that IV ketorolac was no better than IM ketorolac in terms of analgesic efficacy or onset of action (Parke 1995). However, participants who received IM ketorolac required a subsequent analgesic sooner than those who received IV ketorolac. Additionally, the number of patients who achieved a one-point decrease in pain on a 0 to 4 scale after half an hour was greater for IV ketorolac participants than IM ketorolac participants. These differences may have been due to excessively high baseline pain scores, lack of homogeneity in surgery type, and differences in the time of analgesic administration (Parke 1995). Lastly, there were no statistically significant differences in adverse effects between the IV and IM ketorolac groups. Neither group reported any serious adverse events, and no patient was withdrawn early due to an adverse event.
Unfortunately, our analysis of the studies included in this review provided insufficient evidence to support any conclusions about how significantly the risk for adverse effects differs between lower and higher doses of parenteral ketorolac. However, as discussed above, our analysis of the existing literature comparing different doses of IV and IM ketorolac lends credence to the hypothesis that lower doses of parenteral ketorolac may provide equianalgesic effects in comparison to the higher, FDA-approved doses. With this in mind, a healthcare provider could opt for an equally effective lower dose when ADR risk is a clinical concern. It would be worthwhile to conduct further studies regarding the relationship between the occurrence of serious adverse events and different dosing for ketorolac. Specifically, it would be useful to determine whether the FDA-approved doses have a significantly higher occurrence of adverse drug reactions than lower doses with non-inferior analgesic efficacy.
There were various limitations to the present study. This study would have benefited from access to more databases, such as Embase. The inclusion of additional studies contained within databases other than the ones highlighted in our methods may have strengthened our conclusions by decreasing the heterogeneity of the data (as mentioned in our discussion of the IM ketorolac articles) or by allowing for more direct comparisons between IM and IV ketorolac. In addition, there were a number of studies for which we did not have access to the full text. Access to more full article texts would have provided more evidence for this review and allowed for a more impactful conclusion. Moreover, the articles that were reviewed predominantly had inadequate sample sizes. The only article with an adequate sample size (n = 1349) was Yurashevich 2020, which is limited in the clinical implications of its results and conclusions due to its design as a retrospective study. Lastly, because the studies included in our review utilized a variety of different pain scales, directly comparing the results of these studies in a meta-analytical manner is not feasible (Bielewicz 2022).
To establish more definitive, evidence-based conclusions, it will be necessary to perform a large randomized, blinded, and controlled trial with at least 200 participants in each treatment arm with minimal attrition and include both efficacy and ADRs as primary outcome measures (Deschartes 2014, Thorlund 2011).
In conclusion, lower doses of ketorolac 10 mg–30 mg per dose IV/IM may have comparable analgesic efficacy to higher doses ≥30 mg IV/IM and should theoretically lead to a reduction of the occurrence of adverse reactions such as major bleeding. However, more research must be conducted to analyze the full safety profile of higher doses of ketorolac at or above 30 mg IV/IM.
- References
References to studies included in this review
- Duttchen KM, Lo A, Walker A, et al. Intraoperative ketorolac dose of 15mg versus the standard 30mg on early postoperative pain after spine surgery: A randomized, blinded, non-inferiority trial. J Clin Anesth. 2017;41:11-15. doi:10.1016/j.jclinane.2017.05.013
- Folsland B, Skulberg A, Halvorsen P, Helgesen KG. Placebo-controlled comparison of single intramuscular doses of ketorolac tromethamine and pethidine for post-operative analgesia. J Int Med Res. 1990;18(4):305-314. doi:10.1177/030006059001800407
- Eidinejad L, Bahreini M, Ahmadi A, Yazdchi M, Thiruganasambandamoorthy V, Mirfazaelian H. Comparison of intravenous ketorolac at three doses for treating renal colic in the emergency department: A noninferiority randomized controlled trial. Acad Emerg Med. 2021;28(7):768-775. doi:10.1111/acem.14202
- Khadge SD, Tanella A, Lin HM, Ren I, Michaels I, Hyman JB. Retrospective study of the analgesic effect of a 15 mg dose of ketorolac in ambulatory gynecologic surgery. J Clin Anesth. 2020;66:109904. doi:10.1016/j.jclinane.2020.109904
- Minotti V, Betti M, Ciccarese G, Fumi G, Tonato M, Del Favero A. A double-blind study comparing two single-dose regimens of ketorolac with diclofenac in pain due to cancer. Pharmacotherapy. 1998;18(3):504-508.
- Motov S, Yasavolian M, Likourezos A, et al. Comparison of Intravenous Ketorolac at Three Single-Dose Regimens for Treating Acute Pain in the Emergency Department: A Randomized Controlled Trial. Ann Emerg Med. 2017;70(2):177-184. doi:10.1016/j.annemergmed.2016.10.014
- O’Hara DA, Fragen RJ, Kinzer M, Pemberton D. Ketorolac tromethamine as compared with morphine sulfate for treatment of postoperative pain. Clin Pharmacol Ther. 1987;41(5):556-561. doi:10.1038/clpt.1987.71
- Parke TJ, Millett S, Old S, Goodwin AP, Rice AS. Ketorolac for early postoperative analgesia. J Clin Anesth. 1995;7(6):465-469. doi:10.1016/0952-8180(95)00054-l
- Shanechi M, Eke O, Gottlieb M. Comparison of ketorolac dosing in an emergency department setting. CJEM. 2018;20(S2):S74-S77. doi:10.1017/cem.2017.431
- Turner NJ, Long DA, Bongiorno JR, et al. Comparing two doses of intramuscular ketorolac for treatment of acute musculoskeletal pain in a military emergency department. Am J Emerg Med. 2021;50:142-147. doi:10.1016/j.ajem.2021.07.054
- Yee JP, Koshiver JE, Allbon C, Brown CR. Comparison of intramuscular ketorolac tromethamine and morphine sulfate for analgesia of pain after major surgery. Pharmacotherapy. 1986;6(5):253-261. doi:10.1002/j.1875-9114.1986.tb03485.x
- Yoon MH, Yoo KY, Chung SS, Jeong CY, Im WM, Park CJ. Comparative Effects on Postoperative Analgesia According to the Intravenous Dosage of Ketorolac. Korean J Pain. 1995;8(1):43-50.
- Yurashevich M, Pedro C, Fuller M, Habib AS. Intra-operative ketorolac 15 mg versus 30 mg for analgesia following cesarean delivery: a retrospective study. Int J Obstet Anesth. 2020;44:116-121. doi:10.1016/j.ijoa.2020.08.009
- Zhou TJ, Tang J, White PF. Propacetamol versus ketorolac for treatment of acute postoperative pain after total hip or knee replacement. Anesth Analg. 2001;92(6):1569-1575. doi:10.1097/00000539-200106000-00044
Additional references
- Bielewicz J, Daniluk B, Kamieniak P. VAS and NRS, Same or Different? Are Visual Analog Scale Values and Numerical Rating Scale Equally Viable Tools for Assessing Patients after Microdiscectomy?. Pain Res Manag. 2022;2022:5337483. Published 2022 Mar 29. doi:10.1155/2022/5337483
- Castellsague J, Riera-Guardia N, Calingaert B, et al. Individual NSAIDs and upper gastrointestinal complications: a systematic review and meta-analysis of observational studies (the SOS project). Drug Saf. 2012;35(12):1127-1146. doi:10.2165/11633470-000000000-00000
- Dechartres A, Trinquart L, Boutron I, Ravaud P. Influence of trial sample size on treatment effect estimates: meta-epidemiological study. BMJ. 2013;346:f2304. Published 2013 Apr 24. doi:10.1136/bmj.f2304
- Eisenberg E, Berkey CS, Carr DB, Mosteller F, Chalmers TC. Efficacy and safety of nonsteroidal antiinflammatory drugs for cancer pain: a meta-analysis. J Clin Oncol. 1994;12(12):2756-2765. doi:10.1200/JCO.1994.12.12.2756
- García Rodríguez LA, Cattaruzzi C, Troncon MG, Agostinis L. Risk of hospitalization for upper gastrointestinal tract bleeding associated with ketorolac, other nonsteroidal anti-inflammatory drugs, calcium antagonists, and other antihypertensive drugs. Arch Intern Med. 1998;158(1):33-39. doi:10.1001/archinte.158.1.33
- Ketorolac tromethamine – Food and Drug Administration. https://www.accessdata.fda.gov/drugsatfda_docs/label/2014/074802s038lbl.pdf. Accessed June 16, 2022.
- Laska EM, Sunshine A, Marrero I, Olson N, Siegel C, McCormick N. The correlation between blood levels of ibuprofen and clinical analgesic response. Clin Pharmacol Ther. 1986;40(1):1-7. doi:10.1038/clpt.1986.129
- Seymour RA, Ward-Booth P, Kelly PJ. Evaluation of different doses of soluble ibuprofen and ibuprofen tablets in postoperative dental pain. Br J Oral Maxillofac Surg. 1996;34(1):110-114. doi:10.1016/s0266-4356(96)90147-3
- Soleyman-Zomalan E, Motov S, Likourezos A, Cohen V, Pushkar I, Fromm C. Patterns of Ketorolac dosing by emergency physicians. World J Emerg Med. 2017;8(1):43-46. doi:10.5847/wjem.j.1920-8642.2017.01.008
- Thorlund K, Imberger G, Walsh M, et al. The number of patients and events required to limit the risk of overestimation of intervention effects in meta-analysis–a simulation study. PLoS One. 2011;6(10):e25491. doi:10.1371/journal.pone.0025491
- Vadivelu N, Chang D, Helander EM, et al. Ketorolac, Oxymorphone, Tapentadol, and Tramadol: A Comprehensive Review. Anesthesiol Clin. 2017;35(2):e1-e20. doi:10.1016/j.anclin.2017.01.001
- Appendices
7.1. Appendix A: Characteristics of studies
| Study Design | Participants | Outcomes | Results |
|---|---|---|---|
| Duttchen 2017 | |||
| Prospective, randomized, non-inferiority clinical trial | 15 mg IV ketorolac: n = 25; age: 53.0 ± 16; gender: males 68%, females 32%
30 mg IV ketorolac: n = 25; age: 54.0 ± 23; gender: males 68%, females 32% |
Primary outcome: visual analog scale (VAS) pain scores 4 hours after surgery (minimum clinically significant VAS pain score decrease was defined as 18 mm).
Secondary outcomes: morphine usage in the first 8 and 24 hours after the operation. Another secondary outcome was morphine side effects such as sedation, nausea, respiratory depression, etc. |
Mean difference in 4 h VAS pain score between 15 mg vs. 30 mg:
|
| Eidinejad 2020 | |||
| Prospective, double-blind, randomized, non-inferiority clinical trial | 10 mg IV ketorolac: n = 55; age: 40.38 ± 10.82; gender: males 74%, females 26%
20 mg IV ketorolac: n = 55; age: 39.18 ± 9.17; gender: males 80%, females 20% 30 mg IV ketorolac: n = 55; age: 41.64 ± 9.82; gender: males 69%, females 31% |
Primary outcome: alleviation of pain according to the VAS pain score 30 minutes after ketorolac administration.
Secondary outcomes: pain reduction after 15, 45, and 60 minutes following ketorolac administration. Other secondary outcomes included the development of adverse effects and the need for a rescue analgesic after 30 minutes. |
30-minute mean VAS score:
60-minute mean VAS score:
|
| Folsland 1990 | |||
| Randomized, double-blind, parallel trial | 100 mg IM pethidine: n = 27; age: 57.0 ± 16.3; gender: males 59%, females 11%
10 mg IM ketorolac: n = 32; age: 57.4 ± 13.8; gender: males 22%, females 78% 30 mg IM ketorolac: n = 29; age: 54.7 ± 16.8; gender: males 59%, females 41% Placebo: n = 32; age: 57.7 ± 8.4; gender: males 63%, females 38% |
Primary outcome: determine the relative analgesic efficacy and safety of single intramuscular injections of 10 or 30 mg ketorolac, 100 mg pethidine, or placebo patients with moderate, severe, or very severe pain following major surgery requiring abdominal section. |
|
| Khadge 2020 | |||
| Retrospective, non-inferiority trial | 0 mg ketorolac (control): n = 223
15 mg IV ketorolac: n = 112 30 mg IV ketorolac: n = 226 |
Primary outcome: whether intraoperative administration of 15 mg IV ketorolac lowers postoperative opioid administration compared to no ketorolac. Whether there is a difference in effectiveness between 15 mg and 30 mg ketorolac given intravenously. | First pain score
Maximum pain score
Received post-op opioid
|
| Minotti 1998 | |||
| Prospective, double-blind, randomized clinical trial | 10 mg IM ketorolac: n = 60; age: 59 ± 11; gender: males 70%, females 30%
30 mg IM ketorolac: n = 60; age: 62 ± 10; gender: males 75%, females 25% 75 mg IM diclofenac: n = 60; age: 62 ± 9; gender: males 75%, females 25% |
Primary outcome: to assess severity and type of pain at baseline, 30 minutes, 1, 2, 3, 4, 5, and 6 hours after administration. | 30-minute mean NRS score:
60-minute mean NRS score:
|
| Motov 2017 | |||
| Prospective, randomized, non-inferiority clinical trial | 10 mg IV ketorolac: n = 80; age: 41.5 ± 12.1; gender: males 49%, females 51%
15 mg IV ketorolac: n = 80, age: 40.1 ± 12.1, gender: males 40%, females 60% 30 mg IV ketorolac: n = 80; age: 38.8 ± 11.6; gender: males 46%, females 54% |
Primary outcome: numeric rating scale (NRS) pain score 30 minutes after medication administration.
Secondary outcomes: amount of participants experiencing adverse effects and requiring morphine. |
Mean pain reduction:
Mean pain score:
|
| O’Hara 1987 | |||
| Prospective, randomized, double-blind clinical trial | 10 mg IM ketorolac: n = 30; age: 43 ± 14; gender: males 13%, females 87%
30 mg IM ketorolac: n = 31; age: 37 ± 11; gender: males 32%, females 68% 90 mg IM ketorolac: n = 30; age: 43 ± 16; gender: males 23%, females 77% 6 mg IM morphine: n = 30; age: 42 ± 14; gender: males 10%, females 90% 12 mg IM morphine: n = 30; age: 39 ± 12; gender: males 20%, females 80% |
Primary outcome: efficacy and safety of 10, 30, and 90 mg IM ketorolac compared with 6 and 12 mg IM morphine. | Time pain was less than baseline (hr)
|
| Parke 1995 | |||
| Double-blind, randomized, placebo-controlled | 30 mg IV ketorolac: n = 37; age: 59; gender: males 45%, females 55%
30 mg IM ketorolac: n = 38; age: 57; gender: males 50%, females 50% Placebo: n = 37; age: 56; gender: males 59%, females 41% |
Primary outcome: determination of the efficacy and speed of onset of a single dose of IV and IM ketorolac. | Number of patients achieving a one-point decrease of pain within 30 minutes:
|
| Power 1994 | |||
| Double-blind, placebo-controlled, randomized | 30 mg IM ketorolac: n = 25; gender: males 76%, females 24%
10 mg IM ketorolac: n = 25; gender: males 80%, females 20% Placebo: n = 25; gender: males 92%, females 8% |
Primary outcome: determination of the difference in pain relief between 10 mg IM ketorolac, 30 mg IM ketorolac, and placebo. | Withdrawal due to inadequate analgesia:
PCA morphine (24 h, 24 h, mg):
|
| Shanechi 2018 | |||
| Prospective, randomized, double-blind clinical trial | 10 mg IV ketorolac: n = 80
15 mg IV ketorolac: n = 80 30 mg IV ketorolac: n = 80
|
Primary outcome: reduction of pain according to the numeric rating scale (NRS) 30 minutes after medication administration. Difference of more than 1.3 on pain scale = clinically significant.
Secondary outcomes: percentages of people experiencing adverse effects and needing rescue medication. |
Pain score difference from baseline at 30 minutes
|
| Turner 2021 | |||
| Prospective, randomized, single-blind, non-inferiority clinical trial | 15 mg IM ketorolac: n = 55; age: 31.1 ± 9.5; gender: males 53%, females 43%
60 mg IM ketorolac: n = 55; age: 30.7 ± 8.6; gender: males 47%, females 57% |
Primary outcome: change in 1-100 VAS pain score 60 minutes after medication administered.
Secondary outcomes: change in VAS score 30 minutes after administration and reported adverse effects. |
Change in pain score at 60 minutes after medication administration
|
| Yee 1986 | |||
| Double-blind, parallel comparison trial | 10 mg IM ketorolac: n = 48; age: 37.1 ± 11.7; gender: males 35%, females 65%
30 mg IM ketorolac: n = 48; age: 37.1 ± 12.4; gender: males 46%, females 54% 90 mg IM ketorolac: n = 48; age: 37.9 ± 9.7; gender: males 31%, females 69% 6 mg IM morphine: n = 49; age: 36.5 ± 12; gender: males 41%, females 59% 12 mg IM morphine: n = 48; age: 34.1 ± 10.4; gender: males 38%, females 62% |
Primary outcome: evaluate the relative analgesic efficacy and safety of single intramuscular injections of ketorolac tromethamine 10, 30, and 90 mg compared to morphine sulfate 6 and 12 mg in treating of acute postoperative pain. | Overall pain relief:
Sum of Pain Intensity Difference (3 hr, 6 hr):
|
| Yoon 1995 | |||
| Prospective, randomized clinical trial | 10 mg IV ketorolac: n = 16; age: 49.3 ± 3.1; gender: males 56%, females 44%
15 mg IV ketorolac: n = 17; age: 51.0 ± 2.9; gender: males 53%, females 47% 30 mg IV ketorolac: n = 17; age: 53.1 ± 2.8; gender: males 59%, females 41% 45 mg IV ketorolac: n = 17; age: 52.7 ± 2.7; gender: males 53%, females 47% 60 mg IV ketorolac: n = 17; age: 51.9 ± 2.8; gender: males 47%, females 53% Placebo: n = 14; age: 52.1 ± 2.7; gender: males 43%, females 57% |
Primary outcome: analgesic effect according to IV doses of ketorolac. | Pain score (VAS) at 30 minutes after administration:
|
| Yurashevich 2020 | |||
| Retrospective clinical trial | 15 mg IV ketorolac: n = 999; age: 30
30 mg IV ketorolac: n = 350; age: 31 |
Primary outcome: use of opioid in the first 6 hours after surgery.
Secondary outcomes: use of opioid at 24 and 48 hours, average pain score at 6 hours, number of patients with serum creatinine greater than 0.9 mg/dL, number of patients who breastfed within 48 hours of surgery, and use of rescue anti-emetics over the first 48 hours. |
Number of patients who use opioids at 6 hrs post-operation:
Odds ratio 1.13 (95% CI 0.87 to 1.47) |
| Zhou 2001 | |||
| Double-blinded, placebo-controlled study | 2 g IV propacetamol: n = 57; age: 61.4 ± 12.0; gender: males 37%, females 63%
15 mg IV ketorolac: n = 28; age: 64.2 ± 15.3; gender: males 29%, females 71% 30 mg IV ketorolac: n = 27; age: 60.6 ± 11.1; gender: males 22%, females 78% Placebo: n = 52; age: 60.9 ± 12.4; gender: males 40%, females 60% |
Primary outcome: to compare the onset and duration of analgesia and the analgesic efficacy of IV propacetamol (2g) and ketorolac (15 or 30mg) in patients experiencing moderate-to-severe pain after total hip or knee replacement surgery. | Number of patients with “excellent” pain relief during the Global pain evaluation at 6 hours after administration of study medication:
|
7.2. Appendix B: Search strategies
Authors

Timofey Shimko
SCCP-Pacific Treasurer ’22-‘23

Chiron Tran
SCCP-Pacific Historian ’22-‘23

Sophia Wong
SCCP-Pacific President ’22-‘23

Allyson Chan
SCCP-Pacific President ’21-‘22

Anthony Bao
SCCP-Pacific Vice President of Fundraising ’22-‘23

Samantha Seto
SCCP-Pacific Treasurer ’21-‘22
Reviewers
Reviewers report no conflicts of interest.
Dr. Tina Denetclaw
Dr. Patricia Montgomery
Dr. Jade Vitug
 The American College of Clinical Pharmacy is accredited by the Accreditation Council for Pharmacy Education as a provider of continuing pharmacy education.
The American College of Clinical Pharmacy is accredited by the Accreditation Council for Pharmacy Education as a provider of continuing pharmacy education.